Postherpetic neuralgia (PHN) is a debilitating and persistent pain condition that arises as a complication of herpes zoster, commonly known as shingles. This condition occurs when the varicella-zoster virus, which causes chickenpox, reactivates later in life and leads to an outbreak of painful skin rashes.
While the rash and acute symptoms of shingles typically resolve within a few weeks, postherpetic neuralgia can linger for an extended period, significantly impacting the affected individual’s quality of life. In this article, we delve into the intricacies of postherpetic neuralgia, exploring its causes, symptoms, and available treatment options.
Causes and Risk Factors:
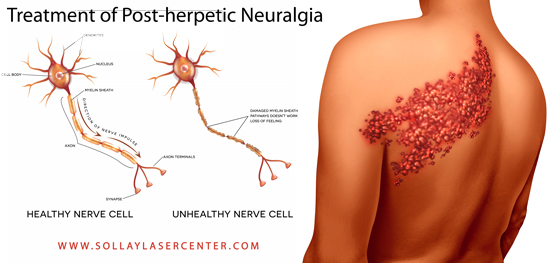
Postherpetic neuralgia is a result of nerve damage or irritation caused by the varicella-zoster virus during a shingles outbreak. The virus remains dormant in the nerve cells after an individual has had chickenpox, and it can reactivate later in life, typically when the immune system weakens with age or due to other health conditions.
Several factors contribute to the development of postherpetic neuralgia, including:
- Age:
- The risk of developing PHN increases with age, particularly in individuals over the age of 60.
- Severity of Shingles Outbreak:
- The more severe the shingles outbreak, the higher the likelihood of developing postherpetic neuralgia.
- Immunosuppression:
- Conditions or treatments that suppress the immune system, such as HIV/AIDS or certain medications, can increase the risk of PHN.
- Pain During Shingles Outbreak:
- Individuals who experience intense pain during the acute phase of shingles are more likely to develop postherpetic neuralgia.
Symptoms:
Postherpetic neuralgia is characterized by persistent and often excruciating pain in the area where the shingles rash occurred. The pain can vary widely in intensity, duration, and quality but is typically described as burning, stabbing, or throbbing. Some common features of PHN include:
- Persistent Pain:
- The pain persists for weeks, months, or even years after the shingles rash has healed.
- Hypersensitivity:
- Affected areas may become hypersensitive to touch, temperature changes, or even the lightest breeze.
- Allodynia:
- Allodynia is a condition where the affected person experiences pain from stimuli that are not typically painful, such as light touch.
- Itching and Numbness:
- Itching and numbness can also be present in the affected area.
- Sleep Disturbances:
- The chronic pain associated with PHN can lead to sleep disturbances, fatigue, and overall reduced quality of life.
Treatment Options:
Managing postherpetic neuralgia requires a comprehensive approach, and treatment aims to alleviate pain, improve function, and enhance the affected individual’s overall well-being. Common treatment options include:
- Antidepressant Medications:
- Tricyclic antidepressants (such as amitriptyline) and certain newer antidepressants (such as duloxetine) are used to help relieve neuropathic pain associated with PHN.
- Anticonvulsant Medications:
- Drug pregabalin 75 mg , commonly used to treat neuropathic pain, can be effective in managing postherpetic neuralgia.
- Topical Treatments:
- Lidocaine patches or creams can provide localized relief by numbing the affected skin and reducing pain.
- Opioid Medications:
- In some cases, opioids may be prescribed for short-term pain relief, but their long-term use is generally avoided due to the risk of dependence and other side effects.
- Nerve Blocks:
- Local anesthetics or steroids may be injected into the affected nerves to provide temporary relief.
- Physical Therapy:
- Physical therapy can help improve flexibility, reduce muscle tension, and enhance overall function.
- Acupuncture and Alternative Therapies:
- Some individuals find relief through acupuncture, biofeedback, or other alternative therapies.
- Lifestyle Modifications:
- Practices such as stress management, adequate sleep, and maintaining a healthy lifestyle can contribute to overall pain management.
Challenges and Complications:
Postherpetic neuralgia poses significant challenges for both patients and healthcare providers. The persistent nature of the pain can lead to emotional distress, anxiety, and depression. Sleep disturbances and fatigue further compound the impact on the individual’s daily life.
Prevention:
While postherpetic neuralgia cannot always be completely prevented, the risk of developing PHN can be reduced through vaccination. The shingles vaccine, which is recommended for individuals over the age of 50, can lower the likelihood of both shingles and its complications, including postherpetic neuralgia.
Conclusion:
Postherpetic neuralgia represents a lingering consequence of the varicella-zoster virus, with its roots in a shingles outbreak. The chronic pain associated with PHN can significantly impair the affected individual’s quality of life, emphasizing the importance of effective management strategies. A multidisciplinary approach, including medication, physical therapy, and lifestyle modifications, is often necessary to address the complex nature of postherpetic neuralgia.
Advances in research and healthcare continue to shed light on new treatment modalities, providing hope for improved outcomes for those grappling with this challenging condition. Ultimately, understanding postherpetic neuralgia and its treatment options is crucial for individuals, healthcare providers, and communities working together to support those affected by this persistent and often burdensome pain syndrome.